GYNECOLOGIC ONCOLOGY SURGEONS EXPERTISE

IS YOUR CANCER SURGEON WORTHY?
Gynecologic Oncologists are the best suited physicians to manage gynecologic cancers. If you are under the care of one of 1000 or so gynecologic oncologists in the country, you have made it past step #1. However, are they all the same and is the one caring for you the best suited for your specialized problem? Well, when this page is indexed by Google enough to where it is widely available it may not be appreciated by some of my colleagues in Gynecologic Oncology. This page addresses the surgical capabilities of gynecologic oncology surgeons that may be taking care of you.
Here is the bottom line. Just like any other profession in this world, everyone does NOT have the same skill base. So, what is safe and what do you need from your surgeon? Here is a chart from a study published in 2004, with the reference noted below. This was a survey of gynecologic oncologists to determine what they feel their skill base is. It is very telling, and in some instances should raise a giant red flag for you in the event that you are seeking very specialized surgery.
Also, to be fair, this chart does NOT address robotic minimally invasive surgery, but we will get to that later. Also, keep in mind that we are now ten years further along the way and unfortunately the surgical expertise deficiencies, particularly in open surgery, have only deteriorated further. I feel I can comment on this more than the average oncologist because I have personally trained over 50 gynecologic oncologists as fellows over the years. The original reference is noted at the end of this article.
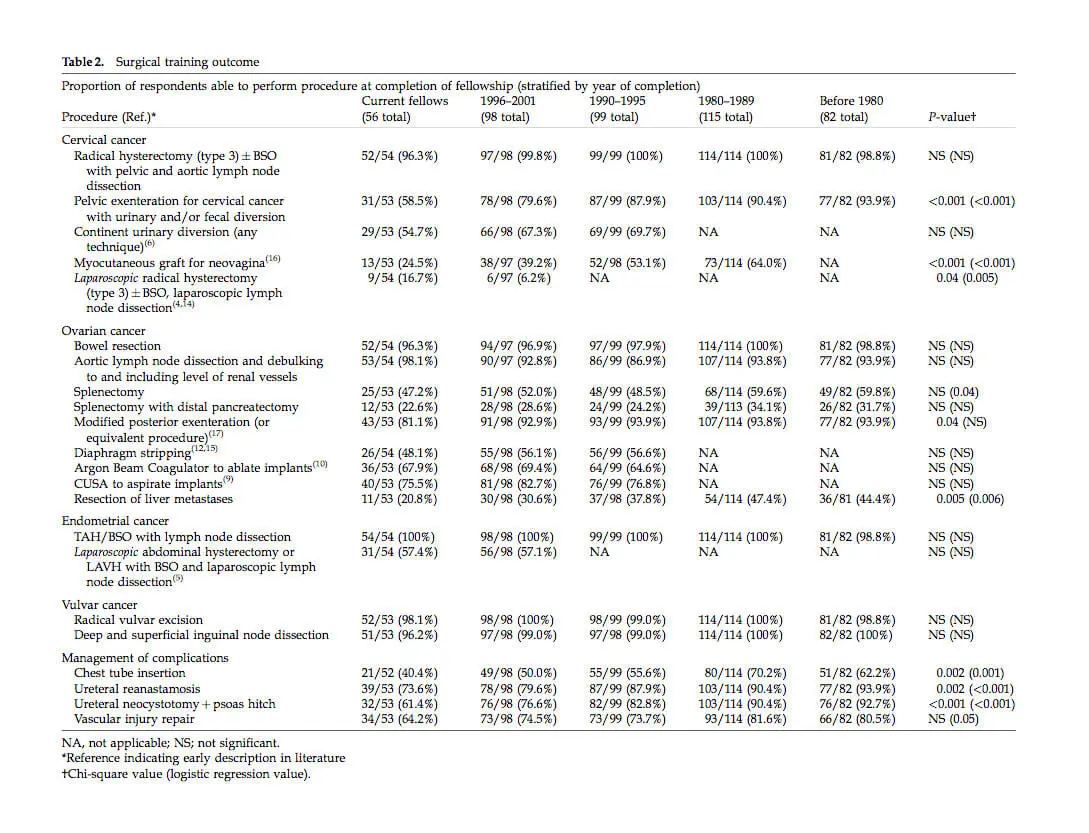
There is an extremely good chance that as of 2015 or thereabouts, you will be treated by someone in the age range represented by the above results table. So, let’s examine the issues practically:
If you need a hysterectomy and basic node dissection, let’s say for endometrial cancer, it appears that as of 2004 the vast majority of gynecologic oncologists could perform this operation using an old fashioned incision. However, it is already disturbing to see that many could not do this comfortably, by their own admission, using minimally invasive surgery which at the time was laparoscopy. The state of the art has jumped quite a bit and many gynecologic oncologist are now trained on the robot, which is a much more advanced technology. The problem is that today’s graduates are probably very comfortable using this technology. But those that trained between 1980 and 2004, who are out there practicing, may have not have benefited from this training in fellowship and are playing catch up. Some have clearly caught up and are leaders in the field. Others have not. All you can do is ask your surgeon and if it seems like a wishy-washy answer, you have the option to get a second opinion.
Moving up the difficulty scale to radical hysterectomy for cervical cancer, it is remarkably unsettling that 4% of gynecologic oncologists trained in recent years do not feel comfortable in performing this type of hysterectomy. The numbers are very small, but is your surgeon one of these? It is also telling that very few felt comfortable performing this operation using laparoscopy. Robotic surgery is an advance that has likely improved this number, but it is still a problem that as of the end of fellowship many practicing surgeons trained between 1980 and 2004 could not perform minimally invasive radical surgery.
Radiation therapy has evolved and is quite good these days. The risk of recurrent cervical cancer is now much lower. However, if you need radical surgery after radiation, you really need to assess whether your surgeon is up for the job. A “standard” pelvic exenteration, which is a last ditch effort to save your life surgically, means removal of most organs in your pelvis and reconstruction thereof. This removal can sometimes be modified to improve quality of life (e.g. no bags for urine or stool) and sexual lifestyle. If one can’t even perform the basic radical operation, the chances that they can perform the modified procedure which requires “out of the box” thinking is almost nil. Reconstruction is crucial for a reasonable lifestyle after exenteration.
Many, if not the majority, of recent graduates cannot perform this surgery. To be fair, in some cases additional surgeons like plastic surgeons, general surgeons, urologic surgeons and so on can be consulted. However, the more surgeons are in the mix the less precise the planned surgery becomes. This is the reason that gynecologic oncology became a specialty some 40-50 years ago. Today, we are reverting back to days of old and the risks of multiple surgeons that you have a good working relationship with must be balanced against the benefits they can provide as a team. Sometimes this can work very well. However, keep in mind, your life and your quality of life which depends upon reconstruction depends upon your surgeon(s). Make sure you have a relationship with each one and the ability to discuss outcomes BEFORE surgery with each one. This is not easy to do if multiple surgeons are involved, but possible. Fortunately, the need for this type of surgery has diminished substantially. BUT if you need it, look carefully for someone who can do it all or can coordinate the team wisely with your wishes in mind.
Ovarian cancer often requires very extensive surgery involving removal of the disease in the pelvis as well as bowel surgery, possible upper abdominal surgery involving removal of spleens, part of the pancreas, part of the liver, removal of the diaphragmatic peritoneum and so on. This is VERY extensive. Why should you care? For every last bit of tumor removed your chances of survival increase substantially. 25 years ago it was acceptable to remove enough tumor to where chunks of half inch (about one centimeter) tumors left behind was reasonable. This was called “optimal cytoreduction”. In some cases, despite the best efforts of the best possible surgeons, this is all that can be achieved. But in the vast majority of cases, most if not all of the visible tumor can be removed using advanced techniques. This, along with better chemotherapy, has made advanced Stage IIIc and Stage IV ovarian, primary peritoneal and Fallopian tube cancer curable in 40- 50% of patients. To achieve this level of surgery, surgeons must be comfortable to remove whatever it takes. Yet, as the table indicates, the majority of graduates in the 21st century can’t perform the upper abdominal procedures required to get the job done. It has only gotten worse. In fact there was a research paper published in October of 2015 in the journal Gynecologic Oncology which suggested that upper abdominal surgery is a “new” concept and requires involvement of other specialists to complete the surgery, because gynecologic oncologists are not trained well for that part of the surgery. Really? That’s news to me. I have been performing whatever it takes to get optimal (often complete) cytoreduction properly done for over 25 years, and was trained for it. Others must have missed that class, I guess. Bottom line? If you are facing advanced stage cancer surgery, get an experienced gynecologic oncology surgeon on your team that can get the job done. Don’t put your life on the line with one that needs to call a bunch of unrelated surgeons who may or may not agree and are also variable in their skill bases.
In the case of vulvar cancer, the surgery required has evolved to “less is more” for good reason, when combined with chemotherapy and radiation. Most surgeons, regardless of when they trained, can perform appropriate surgery and get the job done.
To complete this discussion, robotic surgery has taken center stage in gynecologic oncology surgical management. Assuming a gynecologic oncologist has a good grasp of surgical anatomy, and especially if they have had good open incisional and laparoscopic surgery experience, robotic surgery learning curve is quite fast. Surgeons are up to speed to perform a hysterectomy and node dissection rather quickly, requiring sometimes only a handful of cases to become proficient. Once one moves up the ladder of difficulty to radical hysterectomy, this becomes a steeper learning curve and not all surgeons are ready. In the ultimate surgical difficulty stage of exenteration (i.e. removal of most or all pelvic organs), few surgeons in the country are qualified. At the top of the difficulty scale, when one includes reconstruction, this becomes a very small number of surgeons. All I can say is choose wisely and get as much information as you can from your surgeon. At this level, surgeries are not cookie-cutter “same” and one will not find someone who has done everything possible 1000 times. The best tip I can give is to find a very experienced surgeon for advanced cases, who is generally proficient in open and minimally invasive surgery. For the basics you are probably fine, but if you have a very specialized problem like requiring re-operation for recurrent cancer you may want to get a second opinion.
The more advanced your cancer, the more you would be best served to get an opinion from an experienced surgeon, preferably at a center which performs a lot of similar advanced surgeries. A relationship between surgical volume of surgeons and medical centers has been correlated with better outcomes in many specialities. The more complex the surgery, the more this becomes an issue.
It is always difficult to talk about oneself purely objectively and if you ask around, EVERY surgeon seems to generally think they are the best there is. So, if you are one of my patients how do you know? You can rest assured that the training I have received and the experience I have is unparalleled due to the extent and type of training and practice which is beyond most gynecologic oncologists. This is because my surgical training path was a little different. For example, during ObGyn residency I elected to rotate for as many months as possible on advanced surgical services like the trauma unit at the LA County Hospital. The fellowship I undertook at USC was surgically very intensive as we took care of many very advanced and recurrent cancers in a very under-served population who had their care delayed until advanced stages. Finally, after fellowship I was a member of the surgical oncology division at City of Hope and operated with surgical oncologists, urologic oncologists, vascular surgeons and more on various tumors which had been deemed too advanced for surgery at other medical centers. It was advanced “on the job” training for many years past basic fellowship. The result is that there is very little that I have not seen or complex surgeries that I have not performed multiple times in my career. In fact, I have trained over 50 gynecologic oncologists over the years, who can attest to this. Many are leaders in our field and carry on a strong surgical tradition. I am of course not the only one who has a similar background but, in my opinion, those of us who do are relatively far and few between among the 1000 or so practicing gynecologic oncologists in this country.
Having said all of the above, surgery is not the final answer in treatment of gynecologic malignancies. In some cases, surgery is all one needs to achieve a cure. But in many situations a skillful combination of surgery with use of radiation, chemotherapy, biologicals and integrative support is the key to success. The future will very likely find us in a world of molecular surgery and targeted personalized therapy, obviating the need for radical surgery. Until that day arrives, it might be prudent to carefully select your surgeon on the basis of reputation and training background.
PS. The above is about gynecologic oncologists. If you have another type of cancer there are many oncologic surgeons. There are fellowships for advanced training in surgical oncology, colorectal cancer, breast oncology, urologic oncology and more. The point is that these are all surgeons who received extra training over their general counterparts. In many rural areas you may not have access to one, and in some cases they have enough volume and expertise to be an excellent surgeon for your needs. However, do your research and if possible at least get a second opinion from an oncologic surgeon in a nearby city.
REF and image above are from: 2004 IGCS, International Journal of Gynecological Cancer 14, 23—34